
Another sound, however, indicates a completely different pathology: rales. There, all gas exchange occurs as a result of diffusion and brownian movement.īreath sounds caused by turbulent air flow causing rhonchi and wheezes cannot be heard. In the terminal airways like the bronchioles, there’s little or no air flow. The trachea divides 24 times before it reaches the lung. Rhonchi and wheezes occur in the larger airways and can be heard on both inspiration and expiration. They are moving more air and creating a louder sound, but they’re actually better than before. This explains why patients sometimes sound “worse” after a breathing treatment. Rhonchi are continual low-pitched sounds wheezes are continual high-pitched sounds. The greater the airway obstruction, the higher the pitch. The change in pitch determines whether the sound will be called a rhonchi or a wheeze. In general, the pitch goes up depending on the size of the obstruction, much like a voice does when it goes from a whisper to scream. In a hollow tube, such as the trachea or bronchi, air flows smoothly as long as a patient has no obstructions or “bumps.” When bumps occur, such as globs of mucus, the air must flow around them.Īs air flows around obstructions in the tube, it must change direction and becomes “turbulent.” The air speeds up to go around the obstruction, and the sound it makes-the pitch-changes. We all understand clear breath sounds and know they occur in a healthy tracheobronchial tree. In an unobstructed tube (bronchus), air flows in and out easily and creates a very low-pitched, blowing sound that we equate with clear or healthy breath sounds. Viewing air as “thin” water will help to understand how the sound changes when the flow changes. The sound created is determined by the smoothness or roughness of the flow, much like the difference in the sound of a calm river or a set of rapids.
Adventitious breath sounds rales series#
If we view the bronchial tree as a series of tubes, we’ll see air flows in and out of them either smoothly or turbulently. Sounds have a high and low “pitch” depending on how fast or slow the air moves through the tube (or how many holes you cover up on a flute). When air flows through a tube, it creates a sound. Respiratory therapists need to understand only five breath sounds in everyday clinical practice: clear, rhonchi, wheezes, rales and stridor.
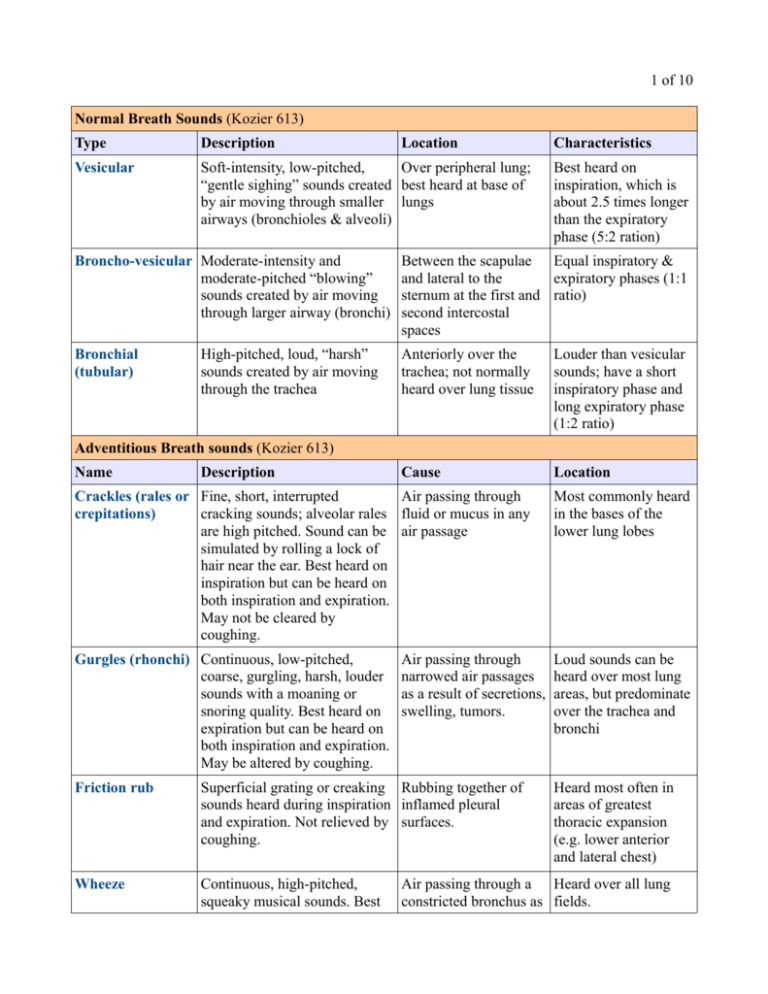
Unfortunately, they’re at the other end of the complicated terminology we learned in school. In the real world, we use adjectives like, “crackles,” “congested,” “squeaky” or “wheezy.” These terms better describe a patient’s condition than do textbook names. Who cares? The goal when assessing breath sounds is to effectively describe what’s going on in the patient’s chest, not to confuse others with descriptions virtually meaningless to anyone except a therapist. Most of us learned breath sounds using complicated terms like “adventitious,” “bronchovesicular” and so on. You’ll need to tune out all other noise and focus on the breath sounds. The key to education: a good teacher the key to listening: concentration. Understanding breath sounds is like understanding music. If you listen carefully, it’s possible to hear all the sounds while at the same time listening to each one: “That’s a flute, that’s a violin, that’s a horn,” or “That’s a wheeze, that’s rhonchi, those are rales.” No lung has just one sound any more than an orchestra or a band has just one instrument. It occurred to me that I do the same thing when I listen to breath sounds. The other day I listened to a concert by the Florida Orchestra and found I could close my eyes and separate the strings from the horns, the woodwinds from the percussion and listen to each section independently. Listening to the ‘Orchestra’ Can Help Determine Medical Status


 0 kommentar(er)
0 kommentar(er)
